How & When to Start Expressing Milk

Pregnancy can be confusing as well as overwhelming. It comes at you out of nowhere and suddenly creates an urge within you to be the world’s best mother to your newborn baby. The first and foremost thing that all mothers have a hard time mastering is Breastfeeding. While it is scientifically and traditionally proven that breast milk and breastfeeding does wonder, some mothers may never have considered expressing milk.
This is because the beautiful and unique bond that the mothers share with their babies while breastfeeding them tells that she may never even need to do so. Whereas a lot of other women may have previously investigated expressing as a feeding option so that their spouse or family members may participate in feeding.
Suppose you have a special gathering where you cannot take your baby along, or you are returning to work, or you are willing to have some time by yourself, or you want to hit the gym, etc. This is where milk expressing comes into play. But a lot of women often ask what is the best time to express milk or when to start expressing milk?
This article will help you clear all your doubts. However, whether you plan to express milk or not, every mother should be equipped with information on expressing milk as an essential component of their antenatal care as well as discharge pack.
What is Expressing Milk
Expressing milk is the process of squeezing out the milk from your breasts in order to preserve it and feed it to your baby later. You can express breast milk by hand, using an electric or manual pump, or both, depending on your preference. You may either give your milk to your baby right away or preserve it in the fridge or freezer once you’ve expressed it.
While we are at it, you must have heard the term Colostrum. It is basically a milky fluid that’s released by the mothers who have given birth recently. It is usually released before breast milk production begins. It entails colostrum expression throughout the last few weeks of pregnancy. It’s also known as “colostrum harvesting” and women are usually recommended to delay commencing this antenatal expression until they are approximately 36 weeks pregnant. Ladies who are expecting numerous births may start earlier because it is more likely for them to give birth earlier than their due date.
Why Express Breast Milk?
You may opt for expressing milk for a variety of reasons like:
- If you had an early delivery and your premature baby has complications post-delivery. In this case, you might not be able to feed them. However, your baby can still feed on your expressed breast milk.
- Someone else can feed your breast milk to your baby if you return to work or school.
- Breastfeeding an adopted baby.
- If you feel that your breasts are engorged or uncomfortably full, expressing milk may help to reduce the discomfort.
- If your baby is unable to suck well.
- If you want to boost your milk production by expressing.
- If you wish to add some breast milk when you start weaning your kid.
If you don’t feel like expressing milk straight away or wonder when can you start expressing milk, wait until you and your baby are comfortable with breastfeeding before beginning to express milk on a regular basis.
How to Express Milk
1. Expressing Breast Milk by Hand
Around 3 to 5 days after your delivery, milk supply increases, and many mothers have a sudden feeling of fullness and engorgement. The pressure and discomfort in your breast at this time might flatten the nipple, making it harder for your baby to latch.
Hand-expressing a small amount of milk softens the nipple and areola, making it simpler for the infant to latch on. Handling engorgement at this preliminary phase is a delicate balancing act; when your milk production grows in volumes, manual expressing is a preferable option.
- Make sure that you wash your hands properly before beginning the process. Keep a sterile feeding bottle, or a wide bowl, or a jug to store the expressed milk.
- Make yourself comfortable in a quiet warm room where you can relax.
- Begin with massaging your breasts gently by starting with long strokes from your armpit to your nipple.
- Proceed with cupping your Breast in a C shape. Make this shape outside your nipple area but not on it. Your thumb and fingers should be in opposite directions.

- Try to feel the texture of the breast and look for something that is rigid in texture. Start to compress or squeeze right from there.
- Change your hand positions on your breasts if you notice that the flow of milk is slowing down. Try to express milk from a different area by placing the thumb and fingers in the same way as directed above.
- Repeat the process with the other breast as well.
2. Expressing Breast Milk with a Pump
Breast pumps (electric or manual) are made to simulate the sucking motion of your baby. The manual version requires you to squeeze the plunger by hand, but the electric version does it for you. It will take a little longer to express milk with a manual breast pump than it will with an electronic pump.
Manual breast pumps have the advantage of being less expensive, easier to operate, lighter in weight, and quieter. Start gently with the suction on the lowest setting if you’re using an electric breast pump. Electric breast pumps have the benefit of doing the job for you and taking less time than manual breast pumps.
The basic procedure of expressing milk with a pump is the same with both manual and electric pumps. It involves the following steps:
- Wash your hands and make sure everything is sterile before use.
- Get comfortable in a quiet warm room and relax.
- Massage your breasts for some time to facilitate the let-down reflex.
- Put the funnel or breast shield of the pump on your nipple.
- For manual breast pumps, after placing them, start pumping slowly. You can expect the milk to start flowing out within a few minutes.
- For electric pumps, after placing the funnel, switch on the machine with a minimum level of speed. You can increase the speed as you notice the milk flow.
- Swap breasts if you notice that the flow of milk is slowing down. Repeat the process.
- Remove the breast shield, put a cap on the bottle, and ensure it’s fastened on correctly once you’ve emptied both breasts. You may either refrigerate it right away or keep it out for at most 4 to 6 hours at room temperature.
- Clean and sanitize the pump and its components.
How to Store Breast Milk
- Breast milk should be stored in sterile containers/bowls/bottles/jugs or specific storage bags.
- The bags should be labeled and dated.
- It would be better for you to store the expressed milk in small amounts to avoid wastage.
- You can then store your breast milk in the following places under the following conditions:
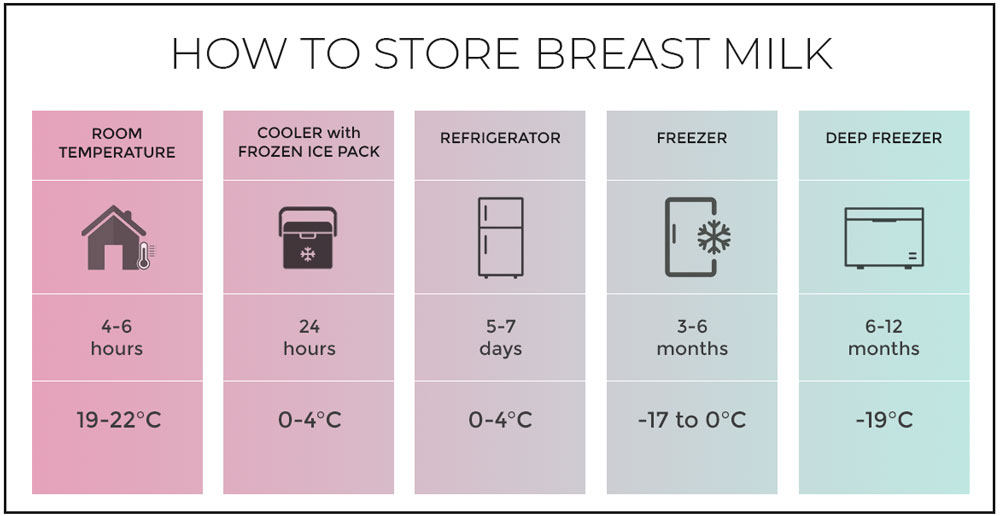
- At room temperature for about 4-6 hours.
- Cooler with frozen ice packs for 24 hours.
- In a refrigerator at 0-4°C or lower for almost a week.
- In the freezer for at most 6 months.
- In a deep freezer for almost a year.
Also read: Dr Brown vs Philips Avent Bottles | In-Depth Comparison
When to Start Expressing Milk
If you wonder when to start expressing milk, we have got you covered. Since you along with your baby are trying to figure out and be comfortable with all the breastfeeding techniques, it is best advised not to start expressing or learning how to express. All of these efforts might make the situations even more complicated than they already are before.
However, a few mothers are advised to start expressing milk within the first few weeks of delivery in case there are breastfeeding difficulties. If this is necessary, your midwife or health visitor will let you know. Otherwise, simply wait and gain comfort and confidence with nursing your newborn first.
If you are planning on expressing milk occasionally
- Then 1 or a few sessions of expressing milk per week would be enough to suit your needs.
- In case you want your significant other to feed your baby daily, try pumping at the same time every day.
- In case you want to express once in a while, say to feed your kid in the evening, you should pump in the morning because a majority of new mothers have an abundance of breast milk output in the morning.
If you are planning on returning to work
- If so, then it’s a great idea to start expressing and storing milk in your freezer ahead of time.
- Starting to express milk around 6 weeks before returning to work is the best way to achieve this as it will enable you to accumulate a substantial volume of backup milk in the freezer without having to express too frequently in a day!
Tips for Expressing Milk
A few tips which would help you while expressing milk are:
- Make yourself comfortable. It would be better to sit in a warm and quiet room for this purpose.
- There is no need to rush. It would be 10 times harder for you to express milk if you would be feeling rushed. Feel no pressure and tension while you are doing it. Every mother and their body is different, so try setting at least 30-45 mins per session when you first begin to express milk. It should take you around 15 to 20 minutes to empty both breasts after you’ve gotten the hang of it.
- Try to relax as much as possible. Keeping a photo or watching a video of your baby might help you feel relaxed and happy. Holding any belonging of your baby like their clothing will also help you relax and in turn help with the milk flow. However, it’s difficult to relax when your infant is sick and in the hospital. Try not to be concerned with how much breast milk you’re making if at all possible; reading a book, listening to music, or watching TV may help to divert you.
Our Advice
Try expressing milk 8-12 times per day including the night session. Your midwife and hospital personnel will be able to assist and support you. The hospital may even have a lactation specialist on staff who can guide you through this. If you wish, you can start using a breast pump once your milk starts flowing.
But you should remember that you will manage to express a few drops of milk when you first start expressing. However, don’t panic because even these droplets are incredibly essential to your baby. It’s is going to be tough, so be patient with yourself and keep trying.

Laura is a trained primary teacher who takes a profound liking in interacting with and bringing out the best in children. She is also an ISSA certified pediatrician with an extensive practice of over 12 years. Laura comprehends the needs of infants and now compresses her expertise into writing thorough parenting guides to aid new parents.






